8 Pancreas and Islet
8.1 Preamble
Pancreas transplantation is undertaken as a treatment for type 1 or insulin-deficient diabetes in two ways:11 Vardanyan M, Parkin E, Gruessner C et al (2010) Pancreas vs. islet transplantation: a call on the future. Curr Opin Organ Transplant 15: 124–130. ×
Either the whole pancreas organ is transplanted,2 or2 White SA, Shaw JA, Sutherland DE (2009) Pancreas transplantation. Lancet 373: 1808–17. ×
The insulin producing pancreatic islet cells are separated from the organ and transplanted.33 Fiorina P, Shapiro AM, Ricordi C, et al. The clinical impact of islet transplantation. Am J Transplant, 2008; 8: 1990–97. ×
There are four units in Australia and one in New Zealand that perform solid organ pancreas transplantation (see Appendix H). The vast majority of solid organ pancreas transplants are undertaken as simultaneous pancreas and kidney (SPK) transplants in recipients with both type 1 diabetes and kidney failure.4 A small minority of transplants are undertaken as solid organ pancreas transplants alone, either after kidney transplantation or in patients with good kidney function who do not require a kidney transplant. There are only a very small number of patients with exceptional circumstances for whom pancreas-alone transplantation is deemed appropriate.2 There are also some patients that require a pancreas transplant along with other organs (for example, combined liver/pancreas, liver/pancreas/kidney, or lung/pancreas transplantation in patients with conditions such as cystic fibrosis). These are uncommon transplant procedures and often referred to as multi-organ transplants.4 Australian and New Zealand Pancreas Transplant Registry Report 1984-2013. Patekar A, Robertson P, Webster A and Chapman J, eds. Australia and New Zealand Pancreas Transplant Registry, Westmead, 2014. ×2 White SA, Shaw JA, Sutherland DE (2009) Pancreas transplantation. Lancet 373: 1808–17. ×
There are two pancreatic islet isolation laboratories in Australia and New Zealand: Westmead Hospital in Sydney and St Vincent’s Institute of Medical Research in Melbourne. Pancreatic islet cell transplantation is currently undertaken at the following infusion centres: Westmead Hospital, St Vincent’s Hospital and Royal Adelaide Hospital.
Simultaneous pancreas (solid organ) and kidney transplantation
As the solid organ pancreas transplant units are national centres with referrals often coming from interstate, patients must first meet broad minimum eligibility criteria to be referred to and undergo subsequent assessment at one of the three units. Further criteria must then be met in order for patients to be entered onto the solid organ pancreas transplant waiting list.
This two-step waitlisting process allows potential recipients to be seen and preliminarily assessed at a transplant unit before their disease progresses to the point that they meet the final criteria for waitlisting for SPK transplantation. This process also minimises the referral of patients who would ultimately be deemed unsuitable for SPK transplantation. The minimum eligibility criteria for referral are based on data demonstrating poor outcomes in subgroups of patients with, for example, significant cardiac disease,5-7 increasing age,8 or obesity.9 Eligibility criteria are also based on feasibility; for example significant bilateral disease of the iliac vessels or marked obesity in the recipient make transplant surgery technically difficult or impossible.9-115 Di Carlo A, Odorico JS, Leverson GE, et al. Long-term outcomes in simultaneous pancreas-kidney transplantation: lessons relearned. Clin Transpl 2003: 215–220. 6 Ma IW, Valantine HA, Shibata A, et al. Validation of a screening protocol for identifying low-risk candidates with type 1 diabetes mellitus for kidney with or without pancreas transplantation. Clin Transpl 2006: 139–46. 7 Sollinger HW, Odorico JS, Becker YT, et al. One thousand simultaneous pancreas-kidney transplants at a single center with 22-year follow-up. Ann Surg 2009; 250(4): 618-30. ×8 Ablorsu E, Ghazanfar A, Mehra S, et al. Outcome of pancreas transplantation in recipients older than 50 years: a single-centre experience. Transplantation, 2008; 86: 1511–14. ×9 Hanish SI, Petersen RP, Collins BH, et al. Obesity predicts increased overall complications following pancreas transplantation. Transplant Proc, 2005; 37: 3564–66. ×9 Hanish SI, Petersen RP, Collins BH, et al. Obesity predicts increased overall complications following pancreas transplantation. Transplant Proc, 2005; 37: 3564–66. 10 Fridell JA, Gage E, Goggins WC, et al. Complex arterial reconstruction for pancreas transplantation in recipients with advanced arteriosclerosis. Transplantation, 2007; 83: 1385–88. 11 Mercer DF, Rigley T and Stevens RB. Extended donor iliac arterial patch for vascular reconstruction during pancreas transplantation. Am J Transplant, 2004; 4: 834–37. ×
Multiorgan transplantation including a solid organ pancreas
These are infrequently performed and will require a collaborative approach involving several transplant centres, each specialising in the specific organs required. As an example, if both a liver and pancreas transplant are required, then the liver transplant centre will be the primary team. They will co-ordinate plans with the centre that performs pancreas transplantation.
8.2 Recipient eligibility criteria
8.2.1 Criteria for referral for solid pancreas transplantation
Patients must be referred to a pancreas transplant unit by their treating nephrologist and/or endocrinologist. Patients will be reviewed by the pancreas transplant unit if they meet the following criteria:
Type I diabetes with insulin dependence
eGFR <30 mL/min
Absence of significant cardiac disease, or adequately treated cardiac disease
Patent iliac vessels bilaterally
Age ideally <50 years (unless medically fit, see below).
In the case of age, individual subjects older than 50 years may still be deemed eligible for solid organ pancreas transplantation if they are otherwise very medically fit.6,8 It must be taken into account, however, that patients generally face a waiting time of approximately two to three years from listing to the time of transplantation. As older age affects the likelihood of a successful outcome from SPK,6,8 alternative transplant options (e.g. kidney alone transplantation, living donor kidney transplantation) also need to be very strongly considered.126 Ma IW, Valantine HA, Shibata A, et al. Validation of a screening protocol for identifying low-risk candidates with type 1 diabetes mellitus for kidney with or without pancreas transplantation. Clin Transpl 2006: 139–46. 8 Ablorsu E, Ghazanfar A, Mehra S, et al. Outcome of pancreas transplantation in recipients older than 50 years: a single-centre experience. Transplantation, 2008; 86: 1511–14. ×6 Ma IW, Valantine HA, Shibata A, et al. Validation of a screening protocol for identifying low-risk candidates with type 1 diabetes mellitus for kidney with or without pancreas transplantation. Clin Transpl 2006: 139–46. 8 Ablorsu E, Ghazanfar A, Mehra S, et al. Outcome of pancreas transplantation in recipients older than 50 years: a single-centre experience. Transplantation, 2008; 86: 1511–14. ×12 Young BY, Gill J, Huang E, et al. Living donor kidney versus simultaneous pancreas-kidney transplant in type I diabetics: an analysis of the OPTN/UNOS database. Clin J Am Soc Nephrol, 2009; 4:845–52. ×
In the case of cardiovascular and/or iliac vessel disease, referral may still be considered if the referring team have a strong expectation that these problems can be significantly resolved. Individual cases may need to be discussed directly with one of the national transplant units before the transplant unit can decide to formally assess the patient’s overall suitability.
8.2.2 Inclusion criteria: solid organ pancreas transplant waiting list
Patients may be referred and assessed if they meet the above criteria for solid pancreas transplantation, however they will not be actively listed for transplantation until they also meet all of the following criteria:
Insulin dependence deemed by the national pancreas transplant unit to be reversible by pancreas transplantation
eGFR <15 mL/min and dialysis impending
Absence of significant cardiac disease, or adequately treated cardiac disease
Patent iliac vessels bilaterally
BMI <35 kg/m² (is a relative contraindication)
Non-smoker or permanent cessation of smoking for more than 3 months (see below).
The expectation that a solid organ pancreas transplant can fully reverse the need for insulin is based on a pattern of insulin deficiency rather than one of insulin resistance (signifying type 1 rather than type 2 diabetes). This is not always straightforward to determine but relies partly on the demonstration of absent or low C-peptide levels (a marker of native insulin production).13,1413 Esmatjes E, Fernandez C, Rueda S, et al. The utility of the C-peptide in the phenotyping of patients candidates for pancreas transplantation. Clin Transplant, 2007; 21: 358–62. 14 Singh RP, Rogers J, Farney AC, et al. Do pretransplant C-peptide levels influence outcomes in simultaneous kidney-pancreas transplantation? Transplant Proc, 2008; 40: 510–12. ×
Smoking has been found to adversely affect transplant outcomes.6,15 For this reason, patients are expected to demonstrate commitment to permanent smoking cessation before they can be transplanted.6 Ma IW, Valantine HA, Shibata A, et al. Validation of a screening protocol for identifying low-risk candidates with type 1 diabetes mellitus for kidney with or without pancreas transplantation. Clin Transpl 2006: 139–46. 15 Biesenbach G, Biesenbach P, Bodlaj G, et al. Impact of smoking on progression of vascular diseases and patient survival in type-1 diabetic patients after simultaneous kidney-pancreas transplantation in a single centre. Transpl Int, 2008; 21: 357–63. ×
While outcomes are significantly improved if patients can be transplanted early in the course of their kidney disease progression,16-18 the limited supply of organs and the needs of the kidney-only waiting list restrict the ability to transplant patients before the point of kidney failure. The majority of patients are transplanted after they commence dialysis (typical eGFR <10 mL/min), however some may receive a transplant just prior to dialysis (10–15%). The ability to transplant patients prior to dialysis is important, as the window of opportunity for transplantation is small for some patients due to the presence of multiple comorbidities. The current mortality rate on the SPK waiting list is approximately 10% per year—significantly higher than age matched patients on the kidney-only waiting list.4,19-2116 Becker BN, Rush SH, Dykstra DM, et al. Pre-emptive transplantation for patients with diabetes-related kidney disease. Arch Intern Med, 2006; 166: 44–48. 17 Grochowiecki T, Szmidt J, Galazka Z, et al. Comparison of 1-year patient and graft survival rates between pre-emptive and dialysed simultaneous pancreas and kidney transplant recipients. Transplant Proc, 2006; 38: 261–62. 18 Mezza E, Grassi G, Dani F, et al. Pre-emptive pancreas-kidney transplantation: multidisciplinary follow-up starts too late. Transplant Proc, 2004; 36: 580–81. ×4 Australian and New Zealand Pancreas Transplant Registry Report 1984-2013. Patekar A, Robertson P, Webster A and Chapman J, eds. Australia and New Zealand Pancreas Transplant Registry, Westmead, 2014. 19 Casingal V, Glumac E, Tan M, et al. Death on the kidney waiting list--good candidates or not? Am J Transplant, 2006; 6: 1953–56. 20 Ojo AO, Meier-Kriesche HU, Hanson JA, et al. The impact of simultaneous pancreas-kidney transplantation on long-term patient survival. Transplantation, 2001; 71: 82–90. 21 Schnitzler MA, Whiting JF, Brennan DC, et al. The life-years saved by a deceased organ donor. Am J Transplant, 2005; 5: 2289–96. ×
8.2.3 Exclusion criteria: solid organ pancreas transplant waiting list
Exclusion criteria for pancreas transplantation are:
Exclusion criteria as per kidney-only transplantation (see Section 5.1.2)
Significant cardiac disease, or inadequately treated cardiac disease
Significant vascular disease
Continuous dual antiplatelet therapy that cannot be safely ceased (in the short term) to allow surgery to proceed (e.g. recent coronary artery stenting at risk of thrombosis); single agent antiplatelet therapy is not an exclusion
Significant psychiatric disease (affecting ability to cope and comply with surgery and treatment)
Ongoing cigarette smoking
Inability to comply with complex medical therapy (e.g. chronic cognitive or neuropsychiatric deficits in the absence of a carer capable of taking on this role)
Addiction to non-prescription illicit drugs (e.g. narcotic or cannabis abuse).
8.2.4 Inclusion criteria: pancreatic islet transplant waiting list
Patients are entered onto the national islet transplant waiting list by recognised Clinical Islet Transplant Programmes. Patients on the national Islet transplant waiting list will be assigned to a recognised Clinical Islet Separation Laboratory by the Clinical Islet Transplant Programme.
Inclusion criteria for pancreatic islet transplantation are:
Type 1 diabetes for five years or more
Severe hypoglycaemic unawareness (documented blood sugar level <3 mmol/l without awareness) that has not responded to optimal conventional insulin therapy, as assessed by an endocrinologist
Age >18
Creatinine clearance >75 mL/min/1.73m²
Serum creatinine <130 umol/L
24 hour urine protein estimation <300 mg/day
Weight ideally <80 kg
The patient has read and signed the islet-specific informed consent form
Absence of donor reactive antibodies by Luminex and virtual crossmatch
Willingness to use effective contraception measures
Ability to understand the protocol and provide informed consent.
8.2.5 Exclusion criteria: pancreatic islet transplant waiting list
Exclusion criteria for pancreatic islet transplantation are:
Weight >80 kg
C-peptide response to arginine (5 g IV)—exclude any patient with C-peptide greater or equal to 0.3 ng/ mL at 2, 3, 4, 5, 7, and 10 minutes post infusion
Creatinine clearance <75 mL/min/1.73 m²
Serum creatinine >130 umol/L
24 hour urine protein estimation >300 mg/day
Baseline haemoglobin <12 g/dL in women or <13 g/dL in men
Baseline liver function tests outside of normal range
Insulin requirement >0.7 IU/kg/day
HbA1c >108mmol/mol (12%)
Serum cholesterol >10 mmol/l
Systemic corticosteroid usage
Treatment with terfenadine, cisapride, astemizole, pimozide, or ketoconazole (that is not discontinued prior to sirolimus administration)
A positive pregnancy test or desire to fall pregnant following islet cell transplantation
Malignant disease other than localised and excised skin squamous cell or basal cell carcinoma
Liver disease, including any form of active viral hepatitis, portal venous abnormality or cirrhosis
Chronic pancreatitis
Significant cardiac disease including ischaemic and valvular heart disease
Respiratory disease including clinically significant asthma, bronchiectasis or obstructive airways disease
Any form of chronic infection that could, viewed by the transplant team, pose a mortality risk after transplantation
Any form of chronic or current acute mental or psychiatric illness that could jeopardise patient safety and adherence to medication in the peri- and post-transplantation period
Allergy to intravenous contrast agents, sirolimus, tacrolimus or anti-thymocyte globulin
Any other disease that in the opinion of the investigator may pose a significant risk to survival or adherence post transplantation.
8.2.6 Retransplantation
SPK retransplantation is technically possible, particularly where an early graft thrombosis has occurred and the pancreas has been removed. Even late failure of both organs might be considered for retransplantation if standard inclusion/exclusion criteria are met. The decision would then have to be made whether to remove both failed organs prior to relisting or at the time of retransplantation.
8.3 Waiting list management
8.3.1 Solid organ pancreas waiting list
Potential transplant recipients are ranked for transplantation according to their referral date and eGFR level. Each solid organ pancreas transplant unit allocates organs to the patient who has been waiting the longest, provided they are suitable and ready for transplantation. Patients are enrolled into OrganMatch by the transplant unit which will enable them to be matched with potential deceased organ donors.
Waiting time is calculated from the date of referral if eGFR is already ≤25 ml/min. Alternatively, if eGFR >25 ml/ min at referral, waiting time only starts once the eGFR is consistently ≤25 mL/min.
Transplantation is only allowed once eGFR is consistently ≤15 ml/min or dialysis has commenced. Of note, because of the typical 2-3 year waiting period, most recipients are transplanted after dialysis has commenced.
Dialysis time itself does not lead to any prioritisation on the waiting list. Although it has been previously shown that more than 12 months pre transplant dialysis detrimentally affects the subsequent pancreas graft survival. However, patients who are highly sensitised to HLA antigens (>75% mPRA) and on dialysis, will be flagged as National Priority and are prioritised nationally in the Kidney Pancreas matching algorithm (see Appendix N). Currently, the logistics of distance make it difficult to include highly sensitised patients from New Zealand in this arrangement.
8.3.2 Islet waiting list
Each islet transplant programme allocates islets to the blood group-matched patient who has been waiting for the longest time on the islet transplant list and is deemed suitable and ready for the islet preparation made available for transplantation. Patients on the waiting list who require a second islet transplant will take priority over those waiting for a first transplant.
Where donor a pancreas meets the appropriate criteria for both solid organ and islet transplantation, it is first offered for solid organ transplantation. If the pancreas is not accepted by the national pancreas transplant units for this purpose, then the pancreas can be offered to the national islet transplant units.
8.3.3 Urgent patients
There is no urgent classification for either solid pancreas or islet transplant candidates.
8.3.4 Histocompatibility Assessment
Each recipient must undergo a series of tests performed at the state Tissue Typing laboratories. These include:
HLA typing using molecular technique such as Next Generation Sequencing (NGS) at the following HLA loci: A, B, C, DRB1, DQB1, DQA1, DPB1, DPA1
HLA antibody screening using Luminex single antigen beads. This screening must have occurred within 120 days to be included in matching. It is optimal that all waitlisted patients are screened every 3 months.
These tests will be used in the histocompatibility assessment by the Tissue Typing labs and in consultation with the clinical unit to assign unacceptable antigens. These assigned unacceptable antigens can assist in excluding a waitlisted patient from incompatible donor offers. Additional comprehensive information is available within the National Histocompatibility Guidelines: https://tsanz.com.au/storage/Guidelines/TSANZ_ NationalHistocompatibilityAssessmentGuidelineForSolidOrganTransplantation_04.pdf
8.4 Donor assessment
8.4.1 Donor information and testing
Table 8.1: Donor information required and donor suitability criteria for solid pancreas donation

Table 8.2: Donor information required and donor suitability criteria for islet cell donation

* Regardless of age, if a donor is accepted for heart, lung, liver and/or kidney donation, then the donor may be accepted for pancreatic islets
8.4.2 Donor suitability criteria
Donor suitability criteria are listed in Table 8.1 and Table 8.2. Similar to the selection process for other organs, donor suitability criteria for pancreas transplantation are based on factors that may adversely impact the success of the procedure,22-26 as well as factors related to recipient safety (e.g. infection risk or transmission of malignancy). DNDD and DCDD donors are suitable for solid organ pancreas transplantation (usually SPK transplantation), although thrombosis rates are higher from DCDD compared with DNDD organs. Within DNDD organs, thrombosis rates are higher in donors over 35 years of age. Currently, islet yields from DCDD donors are insufficient for transplantation, hence these donors are only considered at present for solid organ pancreas donation (in the case of paediatric donors, only DNDD donors are suitable for pancreas donation – see Chapter 11). Suitability criteria for pancreas donation from DCDDs are given in Table 8.3: Extended suitability criteria for pancreas donation after circulatory death.24,2722 Salvalaggio PR, Schnitzler MA, Abbott KC, et al. Patient and graft survival implications of simultaneous pancreas kidney transplantation from old donors. Am J Transplant, 2007; 7: 1561–71. 23 Neidlinger NA, Odorico JS, Sollinger HW, et al. Can ‘extreme’ pancreas donors expand the donor pool? Curr Opin Organ Transplant, 2008; 13: 67–71. 24 Suh N, Ryan B, Allen R, et al. Simultaneous pancreas and kidney transplantation from organ donation after cardiac death. ANZ J Surg, 2009; 79: 245–46. 25 Weiss AS, Smits G and Wiseman AC. Standard criteria donor pancreas donation status is associated with improved kidney transplant outcomes. Clin Transplant, 2009; 23: 732–39. 26 Humar A, Ramcharan T, Kandaswamy R, et al. The impact of donor obesity on outcomes after cadaver pancreas transplants. Am J Transplant, 2004; 4: 605–10. ×24 Suh N, Ryan B, Allen R, et al. Simultaneous pancreas and kidney transplantation from organ donation after cardiac death. ANZ J Surg, 2009; 79: 245–46. 27 D’Alessandro AM, Fernandez LA, Chin LT, et al. Donation after cardiac death: the University of Wisconsin experience. Ann Transplant, 2004; 9:68-71. ×
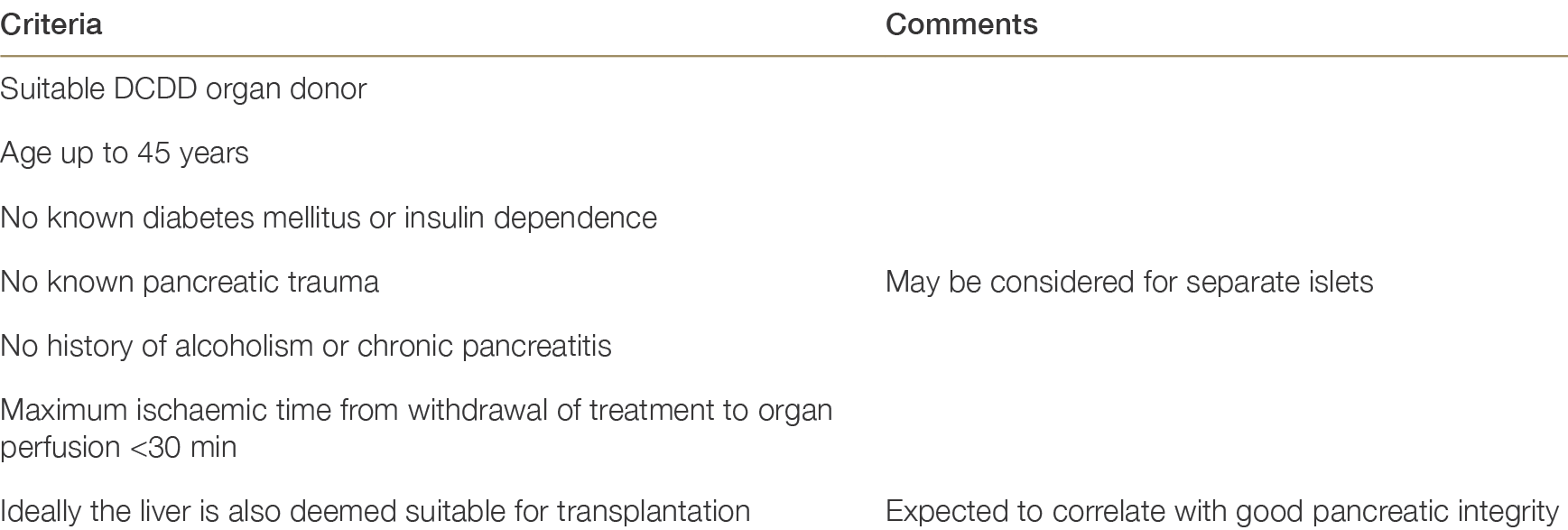
Table 8.3: Extended suitability criteria for pancreas donation after circulatory determination of death24,2724 Suh N, Ryan B, Allen R, et al. Simultaneous pancreas and kidney transplantation from organ donation after cardiac death. ANZ J Surg, 2009; 79: 245–46. 27 D’Alessandro AM, Fernandez LA, Chin LT, et al. Donation after cardiac death: the University of Wisconsin experience. Ann Transplant, 2004; 9:68-71. ×
8.4.3 Organ retrieval
Due to the small number of pancreas transplant units, geographic considerations as well as availability of local expertise need to be taken into account in the process of pancreas retrieval. In some cases the accepting transplant team (the national pancreas transplant unit) will perform the retrieval. Where circumstances make it possible and/or favourable for the local teams to be involved in the process of retrieval and delivery, this will also be considered. Pancreas donations in Western Australia, Queensland and South Australia may involve the local teams, avoiding the need for the staff from the pancreas units to travel interstate for the retrieval process. This process is greatly appreciated by the pancreas transplant units.
8.5 Allocation
8.5.1 General allocation principles
Organ allocation and distribution currently follow processes that have been established over several years based on referral patterns of recipients and geographical considerations regarding retrieval teams and acceptable ischaemic times. The allocation process for pancreas and islet transplantation is reviewed on an ongoing basis.
As stated above (Section 8.3.1), organs are allocated to the blood group identical patient with the longest waiting time who is a suitable recipient and is currently active on the waiting list. In OrganMatch , the kidney/ pancreas and pancreas algorithm is used to determine the potential list of recipients from which the transplant units will select the most suitable recipient (Appendix N). Occasionally allocation may deviate from this general rule if, for example, the donor is very small and the intended recipient is very large, or vice versa. Similarly, where the donor is DCDD or higher-risk—necessitating a short cold ischaemia time—and the recipient cannot reach the transplant unit in time, an alternative recipient may have to be chosen.
Very rarely, a patient on the waiting list who is at risk of death from either hypos or lack of dialysis access may be given priority irrespective of waiting time. There is no official definition of an urgent category for this type of pancreas transplant within Australia and New Zealand.
Patients on the waiting lists are reviewed annually by the pancreas transplantation teams, either by a transplant physician or transplant surgeon. Normally this occurs at an interstate clinic, but occasionally will necessitate the patient travelling to the transplant centre where they are listed.
8.5.2 Organ sharing and rotation
Donor pancreata arising in New Zealand are initially offered to the Auckland National Pancreas Transplant Unit. If the Auckland Unit is unable to use the organs (e.g. no suitable recipient currently listed, lack of availability of appropriate surgeons for either the retrieval or transplant procedure) then the Australian Pancreas Transplant Units (Westmead, Monash, Royal Adelaide) may receive the offer. For logistical reasons it would be rare for this to happen.
In Australia, organs will initially be considered for sensitised recipients that are listed nationally. If there are no suitable recipients, then organs will be allocated using established geographic patterns of referral as follows:

Donor pancreata arising in New South Wales, Australian Capital Territory, Queensland and Western Australia are initially offered to the Westmead National Pancreas Transplant Unit for consideration for simultaneous kidney and pancreas transplantation. If the Westmead Unit is unable to use the organs (e.g. no suitable recipient currently listed, lack of availability of appropriate surgeons for either the retrieval or transplant procedure due to simultaneous pancreas donor or transplant) then the Monash and Royal Adelaide Units will receive the offer, followed by the islet units (Westmead followed by Victoria/South Australia).
Donor pancreata arising in Victoria or Tasmania are initially offered to the Monash National Pancreas Transplant Unit for consideration for simultaneous kidney and pancreas transplantation. If the Monash Unit is unable to use the organs (e.g. no suitable recipient currently listed, lack of availability of appropriate surgeons for either retrieval or transplant procedure) then the Westmead and Royal Adelaide Units will receive the offer, followed by the the islet units (Victoria/South Australia and Westmead).
Donor pancreata from South Australia and Northern Territory will initially be offered to the Royal Adelaide Unit for consideration for simultaneous kidney and pancreas transplantation. If the Royal Adelaide is unable to use the organs (e.g. no suitable recipient currently listed, lack of availability of appropriate surgeons for either retrieval or transplant procedure) then Westmead and Monash will receive the offers on rotation. When all centres decline the pancreas for solid transplant, the pancreas is offered back to Royal Adelaide for islet transplantation, followed by Victoria and New South Wales.